By A correspodent
In an age of health influencers and viral remedies, the conversation around headaches—one of the most common neurological complaints globally—has taken a life of its own. From salt water “cures” to claims about brain painlessness, widely circulated theories often blur the line between science and speculation. But what does medical research actually say?
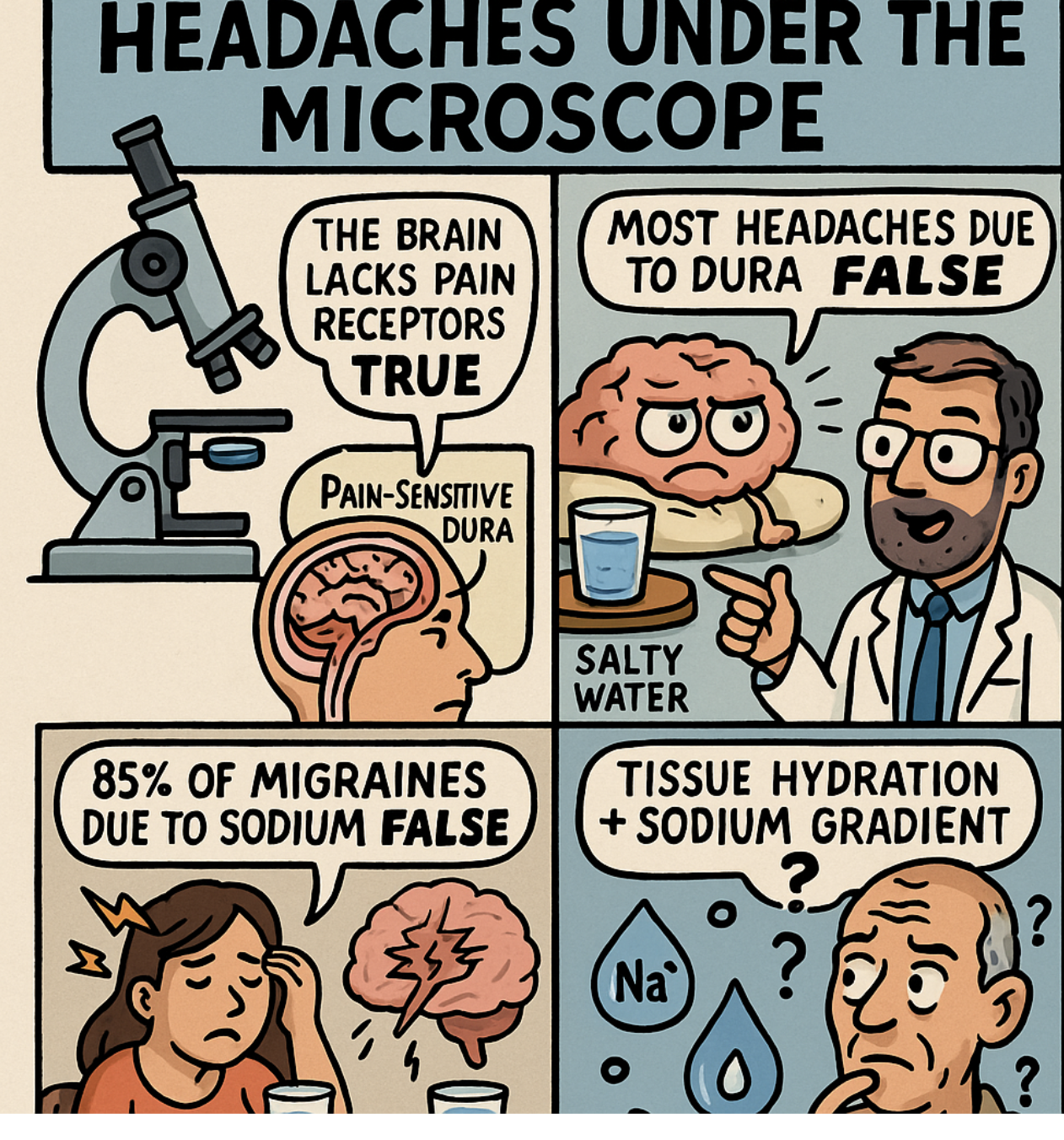
This feature examines four widely shared assertions about headache origins and treatment:
- That most headaches originate from the dura mater due to stretching or contraction.
- That brain surgery is painless because the brain lacks pain receptors.
- That 85% of migraines stem from sodium deficiency, allegedly reversible with salt water.
- That tissue hydration and headache relief are linked to the sodium gradient.
By unpacking decades of neurophysiology, pain science, and clinical studies, we seek clarity behind the claims.
The Brain’s “Silent Core” — But Not So Silent After All
Let’s begin with what’s true: the brain parenchyma itself cannot feel pain. It lacks nociceptors—the specialized sensory neurons that detect pain. That’s why neurosurgeons can perform procedures on awake patients without causing pain, a fact frequently cited to explain why “brain surgery is painless.”
But this truth, while accurate, can be misleading. The brain doesn’t float in a vacuum. It’s wrapped in layers—the meninges—that are very much pain-sensitive. In particular, the dura mater, the outermost layer, is densely innervated by branches of the trigeminal and cervical nerves, making it a key player in many types of headaches.
Patients undergoing awake craniotomies often report pain when surgeons touch or manipulate the dura. Even the pia mater (the delicate innermost layer) and dural blood vessels can contribute to pain perception. So while the brain tissue itself may be “silent,” its surrounding structures speak volumes when irritated.
Stretch, Contract, Scream? Debunking the Dura Myth
One popular narrative claims that “most headaches are caused by stretching or contracting the dura mater.” This idea has some basis—but it oversimplifies a vastly more complex picture.
Studies confirm that mechanical stress on the dura, whether from spinal instability, tumors, or increased intracranial pressure (ICP), can provoke pain. The myodural bridge—a connection between neck muscles and the dura—is one such anatomical culprit behind cervicogenic headaches. Similarly, hydrocephalus, aneurysms, or arterial pulsations can stretch the dura and cause pain.
Yet, attributing most headaches to this mechanism is misleading. Tension-type headaches are typically linked to muscle contraction in the neck and head. Migraines, on the other hand, involve the trigeminovascular system, neurogenic inflammation, and vascular dysregulation, with the dura playing a secondary role. Occipital neuralgia, cluster headaches, and medication overuse headaches all stem from different origins.
In short, the dura contributes, but it’s just one note in a broader neurological symphony.
Salt Water and Sodium: Miracle Cure or Misguided Trend?
Social media is awash with claims that 85% of migraines are due to sodium deficiency—and that a glass of salt water can bring “permanent remission.” Compelling? Perhaps. Clinically verified? No.
In a review of the literature, no scientific evidence supports this 85% figure. It appears to be anecdotal at best. Some studies, like a 2016 analysis from NHANES, found an inverse correlation between sodium intake and self-reported migraine history—suggesting that people who consumed more sodium had fewer migraines. But this is not causation. And other studies suggest the opposite: that high sodium may trigger or worsen headaches, especially in those with hypertension.
Moreover, a lower sodium diet (like the DASH diet) has been linked to reduced headache risk in general. Salt water might help in specific cases of dehydration or electrolyte imbalance, but as a universal remedy, it’s unsupported—and potentially harmful for those with cardiovascular risk.
Hydration, Osmosis, and Head Pain: A Real Link, But Not That Simple
Where the sodium narrative holds some water—pun intended—is in the role of hydration. Dehydration is a well-documented trigger for various types of headaches, including migraines. Low fluid intake can lead to cellular shrinkage, increasing mechanical tension on brain-supportive structures.
Sodium plays a vital role in this process. It is the main extracellular ion and influences osmotic gradients—the forces that govern fluid movement into tissues. A functioning sodium-potassium pump maintains this gradient, and when it falters (due to illness, poor diet, or overhydration), it can disrupt cellular function.
So yes, tissue hydration and sodium balance are important for neurological stability. But that doesn’t mean drinking brine is the answer. The body maintains a tight homeostatic control over sodium levels; even minor imbalances can have wide-ranging effects, including on blood pressure and renal function.
The idea that salt water “restores the sodium gradient and relaxes the dura” oversimplifies a complex system. In fact, the body’s baroreceptors, kidneys, hormones like aldosterone, and vasculature all interact to regulate sodium and water distribution.
Conclusion: From Myth to Medicine
When it comes to headaches, the truth lies somewhere between neurology textbooks and lived experience. Here’s where the science lands on the four claims:
- ✅ The brain lacks pain receptors: True for the parenchyma, but the meninges and blood vessels are pain-sensitive.
- ⚠️ Most headaches are due to dura stretching/contraction: Mechanistically plausible for some types, but not most. Headaches have diverse and multifactorial origins.
- ❌ 85% of migraines are due to sodium deficiency: No credible scientific support. Sodium may play a role in select cases, but this claim is unverified and overstated.
- ⚠️ Tissue hydration and sodium gradient affect headache: Partially true. Hydration and sodium balance are important, but the pathway from salt water to headache relief is far more nuanced than claimed.
Medical Advice? Seek a Professional, Not a Post
For those suffering frequent or debilitating headaches, the best course is not self-diagnosis or saltwater remedies, but a thorough clinical evaluation. Treatment may involve medication, lifestyle changes, hydration, stress management, or even dietary modifications—but only when guided by a medical professional.
The brain may not feel pain—but misinformation about it certainly can cause harm.
